What is dialysis?
Dialysis is a treatment for people whose kidneys are failing. When you have kidney failure, your kidneys don’t filter blood the way they should. As a result, wastes and toxins build up in your bloodstream. Dialysis does the work of your kidneys, removing waste products and excess fluid from the blood.
Who needs dialysis?
People who have kidney failure, or end-stage renal disease (ESRD), may need dialysis. Injuries and conditions like high blood pressure, diabetes and lupus can damage kidneys, leading to kidney disease.
Some people develop kidney problems for no known reason. Kidney failure can be a long-term condition, or it can come on suddenly (acute) after a severe illness or injury. This type of kidney failure may go away as you recover.
There are five stages of kidney disease. In stage 5 kidney disease, healthcare providers consider you to be in end-stage renal disease (ESRD) or kidney failure. At this point, kidneys are carrying out around 10% to 15% of their normal function. You may need dialysis or a kidney transplant to stay alive. Some people undergo dialysis while waiting for a transplant.
Procedure Details
What are the types of dialysis?
There are two ways to get dialysis:
Hemodialysis.
Peritoneal dialysis.
What is hemodialysis?
With hemodialysis, a machine removes blood from your body, filters it through a dialyzer (artificial kidney) and returns the cleaned blood to your body. This 3- to 5-hour process may take place in a hospital or a dialysis center three times a week.
You can also do hemodialysis at home. You may need at-home treatments four to seven times per week for fewer hours each session. You may choose to do home hemodialysis at night while you sleep.
What happens before hemodialysis?
Before you start hemodialysis, you’ll undergo a minor surgical procedure to make it easier to access the bloodstream. You may have:
Arteriovenous fistula (AV fistula): A surgeon connects an artery and vein in your arm.
Arteriovenous graft (AV graft): If the artery and vein are too short to connect, your surgeon will use a graft (soft, hollow tube) to connect the artery and vein.
AV fistulas and grafts enlarge the connected artery and vein, which makes dialysis access easier. They also help blood flow in and out of your body faster.
If dialysis needs to happen quickly, your provider may place a catheter (thin tube) into a vein in your neck, chest or leg for temporary access.
Your provider will teach you how to prevent infections in your fistula or graft. This provider will also show you how to do hemodialysis at home if you choose to do so.
What happens during hemodialysis?
During hemodialysis, the dialysis machine:
Removes blood from a needle in your arm.
Circulates the blood through the dialyzer filter, which moves waste into a dialysis solution. This cleansing liquid contains water, salt and other additives.
Returns filtered blood to your body through a different needle in your arm.
Monitors your blood pressure to adjust how fast blood flows in and out of your body.
What happens after hemodialysis?
Some people experience low blood pressure during or immediately after hemodialysis. You may feel nauseous, dizzy or faint.
Other side effects of hemodialysis include:
Chest pain or back pain.
Headaches.
Itchy skin.
Muscle cramps.
Restless legs syndrome.
What is peritoneal dialysis?
With peritoneal dialysis, tiny blood vessels inside the abdominal lining (peritoneum) filter blood through the aid of a dialysis solution. This solution is a type of cleansing liquid that contains water, salt and other additives.
Peritoneal dialysis takes place at home. There are two ways to do this treatment:
Automated peritoneal dialysis uses a machine called a cycler.
Continuous ambulatory peritoneal dialysis (CAPD) takes place manually.
What happens before peritoneal dialysis?
About three weeks before you start peritoneal dialysis, you’ll have a minor surgical procedure. A surgeon inserts a soft, thin tube (catheter) through your belly and into the peritoneum. This catheter stays in place permanently.
A healthcare provider will teach you how to perform peritoneal dialysis at home and prevent infections at the catheter site.
What happens during peritoneal dialysis?
During peritoneal dialysis, you:
Connect the catheter to one branch of a Y-shaped tube. This tube connects to a bag that has dialysis solution. The solution flows through the tube and catheter into the peritoneal cavity.
Disconnect the tube and catheter after about 10 minutes, when the bag is empty.
Cap off the catheter.
Go about your usual activities while the dialysis solution inside the peritoneal cavity absorbs waste and extra fluids from the body. This process can take 60 to 90 minutes.
Remove the cap from the catheter and use the other branch of the Y-shaped tube to drain the fluid into a clean, empty bag.
Repeat these steps up to four times a day. You sleep with the solution in your stomach all night.
Some people prefer to do peritoneal dialysis at night. With automated peritoneal dialysis, a machine called a cycler pumps the fluid in and out of the body while you sleep.
What happens after peritoneal dialysis?
The liquid in your belly can make you feel bloated or full. It might feel uncomfortable, but the treatment isn’t painful. Your stomach may stick out more than usual when it’s filled with fluid.
Risks / Benefits
What are the potential risks or complications of hemodialysis?
Some people have problems with the AV fistula or graft. You may develop an infection, poor blood flow or a blockage from scar tissue or a blood clot.
Rarely, the dialysis needle comes out of your arm, or a tube comes out of the machine, during dialysis. A blood leak detection system alerts you or the medical staff to this problem. The machine temporarily shuts off until someone fixes the problem. This system protects you from blood loss.
What are the potential risks or complications of peritoneal dialysis?
Some people develop skin infections around the catheter. You’re also at risk for peritonitis, an infection that occurs when bacteria get inside the abdomen through the catheter. You may experience fever, abdominal pain, nausea and vomiting.
Using the abdominal catheter and pumping your belly full of fluid can weaken abdominal muscles over time. You may develop a hernia. This condition occurs when an organ like the small intestine pokes through the abdominal muscles. You may feel a bulge near the belly button or in the groin area between the abdomen and upper thigh. Your doctor can repair a hernia with surgery.
During peritoneal dialysis, your body absorbs dextrose, a sugar, from the dialysis solution. Over time, this extra sugar can lead to weight gain.
Recovery and Outlook
What’s the outlook (prognosis) for someone on dialysis?
It’s possible to live 10 to 20 years on dialysis. The outlook varies depending on your age, overall health, the cause of kidney failure and other factors. If you get a kidney transplant, you can stop dialysis when your new kidney starts working.
Will I have activity restrictions while I’m on dialysis?
Many people on dialysis continue to live active lives, working, raising families and traveling. When you travel, your healthcare provider can help arrange for you to get dialysis at a center at your new location. If you’re doing either type of self-dialysis, you can take dialysis solution bags and the portable home dialysis machine (if needed) with you.
People who use peritoneal dialysis may need to limit exercise or certain physical activities when the abdomen fills with dialysis solution. Otherwise, exercise is typically OK for people on dialysis. You should ask your provider about participating in specific activities or sports.
When to Call the Doctor
When should I call the doctor?
You should call your healthcare provider if you experience:
Difficulty urinating.
Dizziness, fainting, unusual thirst (dehydration) or other signs of low blood pressure.
Nausea and vomiting.
Signs of infection, such as fever or oozing and redness at the AV fistula or catheter site.
Severe abdominal pain.
Unusual bulge in the abdomen or groin (hernia).
Products and reference designs of Dialysis machine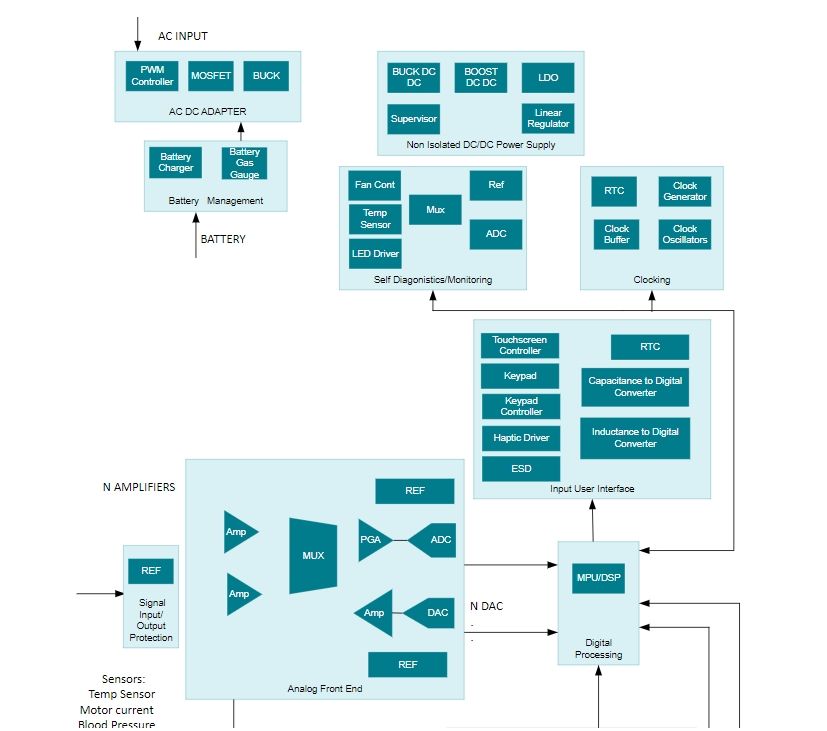
AC/DC adapter
The AC/DC adapter subsystem converts the AC power lines to an isolated regulated DC output. Typically this is a AC/DC adapter which is a standalone unit. AC/DC adapter includes PWM controllers、Isolated DC/DC converters & modules, the Corresponding products are UCC2813-1、LM5018
Non-isolated DC/DC power supply
The non-Isolated power supply subsystem provides the point-of-load power for devices including processors, analog circuitry, etc. LED driver for driving the photo-optical sensors. Non-isolated DC/DC power supply includes Buck converters (integrated switch)、Linear & low-dropout (LDO) regulators、Isolated DC/DC converters & modules, the Corresponding products are LMR51450、TPS7A11、LM5018
Battery management
Energy Storage Subsystem performs Gas Gauging while charging the battery. Battery management includes Battery charger ICs, the Corresponding products are BQ24050、BQ25731
Self-diagnostics/monitoring
Self-diagnostics/Monitoring subsystem includes the temperature sensing and control, LED driver to drive the LEDs which indicate the status, ADCs to convert the results to digital data, MUX for multiplexing etc. Self-diagnostics/monitoring includes Precision ADCs, the Corresponding products are ADS124S08、ADS7028、ADS7828
Clocking
The clock subsystem consists of real-time-clock, clock frequency generation with buffers and clock distribution. Clocking includes Real-time clocks (RTCs) & timers, the Corresponding product is LMC555
Input user interface
The Input User Interface subsystem includes a keypad, keypad controller, ADC to digitize the bar code sensor output, touchscreen controller, Capacitance-to-digital converters, Inductance-to-digital converters, haptic driver etc. Input user interface includes Signal conditioners、Touchscreen controllers, the Corresponding products are LMP91000、TSC2007
Signal input/output protection
Signal Input/Output Protection Subsystem protects the sensor and analog front end from ESD damage. Signal input/output protection includes ESD protection diodes, the Corresponding products are TPD4E1U06、TPD4E001、TPD4S009
Analog front end
The Analog front-end subsystem incorporates op amps as gain stages, programmable gain stages and filters, multiplexers, and ADCs to produce digitized output using the outputs of the photo optical/electrochemical sensors , so that they can be processed by the system processor. A digital-to-analog converter (DAC) is often used to calibrate the sensor amplifiers to maximize the sensitivity of the electrodes. Analog front end includes Analog switches & muxes、General-purpose op amps、Instrumentation amplifiers, the Corresponding products are TMUX2889、TLV9061、INA819
Digital processing
The digital processing subsystem includes control of the system and processing of sensing signals. Digital processing includes C2000 real-time microcontrollers, the Corresponding products are TMS320F28P659DK-Q1、TMS320F2800155-Q1、TMS320F2800153-Q1
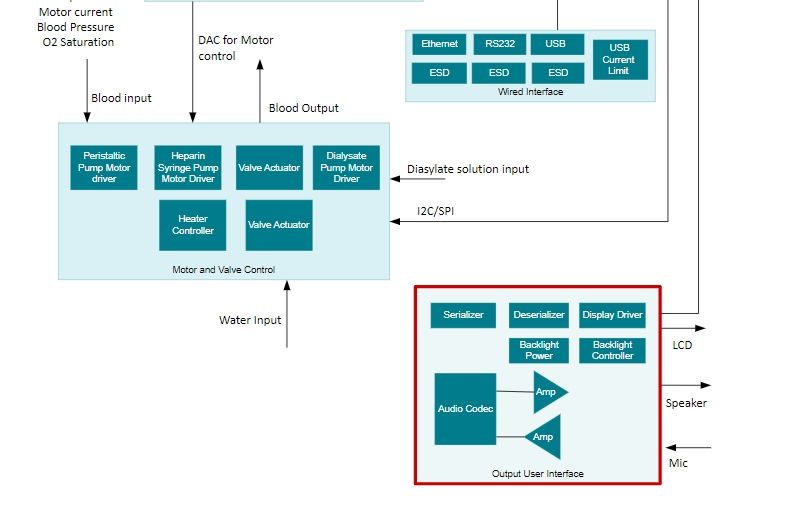
Wired interface
The wired interface subsystem is used to connect the system to a computer for data transfer through various interfaces like USB, Ethernet, RS-232. Wired interface includes RS-232 transceivers、Ethernet PHYs, the Corresponding products are TRS3122E、DP83848H
Motor & valve control
Isolated Gate drivers, FETs, Diagnostics, Protection, (Relay, Thyritors, IGBTs). Motor & valve control includes Brushed DC (BDC) motor drivers、Solenoid drivers、Analog current-sense amplifiers, the Corresponding products are DRV8412、DRV104、INA280
Output user interface
The output user interface subsystem consists of display, printer etc. Output user interface includes Backlight LED drivers、LVDS, M-LVDS & PECL ICs、FPD-Link SerDes, the Corresponding products are TPS92360、SN65LVDS179、DS90UB914A-Q1
A note from Cleveland Clinic
Dialysis is a lifesaving treatment for people with kidney failure or end-stage renal disease (ESRD). You may stay on dialysis indefinitely or just until you can get a kidney transplant. There are different types of dialysis. Some people prefer to do dialysis at home, while others want to go to a hospital or dialysis center. Your healthcare provider can review dialysis options with you to find the treatment that works best for you.
Previous: Electric power steering (EPS)